When menstrual pain strikes, many women use the painkillers they have in their medicine boxes. However, experts have discovered that stronger painkillers like the non-steroidal anti-inflammatory drugs may be more effective than paracetamol for menstrual pain.
When it is that time of the month, most women know that menstrual cramps will come. It starts with pain in their lower abdomen, which spreads to the lower back and their inner thighs. The pain could be so bad that it might warrant staying off school.
Menstrual cramps, or dysmenorrhea (as physicians call it), are one of the most common healthcare problems that women suffer during their reproductive years. It has been estimated that as many as 30 to 50 per cent of all women suffer from pain during their menstrual period, with the incidence being highest in younger women, from teenagers to women in their 30’s.
In fact, at least 10 per cent of younger women have symptoms so severe that they are unable to handle their normal range of activities, and miss days of work and important social functions because any movement or activity is too painful. Usually, for the first day or two of menstruation, only bed rest is tolerable until the symptoms finally pass.
Period pain is thought to be caused by an excess or imbalance of certain hormones released by the body during menstrual periods, including one called prostaglandin.
Besides the lower back pain, other problems that these women experience such as headaches, mood swings, bloating and breast tenderness could be so severe that women with cramps regard their monthly period with apprehension and even dread.
Despite the many symptoms and the millions of sufferers, menstrual cramps have been traditionally considered by the medical community to be a “minor” female ailment. The problem was either ignored or else treated with powerful painkilling drugs and tranquilizers.
Luckily, the medical community’s interest in menstrual cramps has increased during the past two decades. Researchers’ understanding now of what causes menstrual cramps has led to newer, much more effective drug treatments, as well as nutritional and other lifestyle-related therapies.
Moreover, the latest Cochrane review on what works best in alleviating period pain found out that non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin may be more effective than paracetamol to relieve this pain.
The medications, collectively known as non-steroidal anti-inflammatory drugs (NSAIDs), are widely used for various aches and pains, but it has been unclear whether they are as effective as acetaminophen — the active ingredient in common painkillers such as paracetamol and a number of products marketed specifically for menstrual symptoms.
The updated review included data from 73 trials carried out in 18 different countries and involving a total of 5,156 women. The trials compared NSAIDs with placebo, with each other, and with paracetamol.
The review showed that NSAIDs are very effective for treating period pain compared with placebo. This applied to all NSAIDs tested except aspirin, for which there was only limited evidence of effectiveness.
Although a large number of different NSAIDs were tested in the trials, no one drug emerged as more safe or effective than the rest. Nevertheless, exactly why they might be even more effective than acetaminophen is unclear.
All women that experience menstrual cramps needed to see a medical doctor to decide what was responsible for the pain. There are two types of menstrual pain; primary dysmenorrhea and secondary dysmenorrhea.
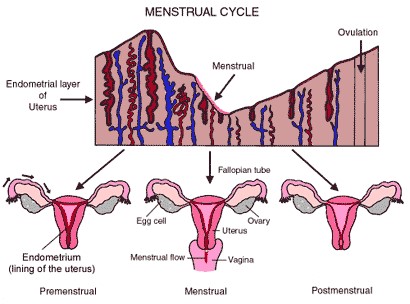
The primary dysmenorrhea is like a normal component of menstrual flow because, usually, it is mild. The pain comes a few hours or days before the menstrual flow and ceases immediately the menses starts to flow. It indicates that, for that month, that woman actually ovulated.
The secondary dysmenorrhea, which is also referred to as congestive dysmenorrhea, is a period pain that is due to one kind of disease condition or the other. These include fibroid, pelvic infection and other forms of pelvic problems such as pelvic tumour.
When the period pain is due to primary dysmenorrhea, reassurance and painkillers are usually the recipe, whereas congestive dysmenorrheal would need further investigation to know what exactly was responsible and treat it appropriately.


